All about your cat's dental health
When Ralph Wiggum told Lisa Simpson that his cat's breath smelled like cat food, he didn't know how lucky he was. Because cat breath can smell a lot more like... well, let's just say it can smell bad, really, really bad. But it doesn't have to!
Inside your cat's mouth
Cats' mouths have unique anatomy.
First, the tongue. Your cat's tongue is covered in little barbs called papillae. These point backwards enabling your cat to rasp meat off bones and catch dirt and loose hair while grooming. Although these barbs are very good for fur cleaning, because they point backwards anything that gets stuck to them tends to get swallowed. This is why cats get fur balls. It's also why they are at risk of things like string foreign bodies. Once something gets caught on the barbs, it can't be spat out. Shame this doesn't apply when you give your cat a tablet!
Next, the teeth. Cats have far fewer but much sharper teeth than dogs. Adult cats have 30 teeth (dogs have 42). But like dogs, cats have different teeth for different purposes. They have:
- incisors for nibbling meat off bones and fleas out of fur
- canines for grabbing and puncturing
- premolars for chewing and tearing
- molars for crushing (bones and biscuits)
The canine teeth in cats have grooves down the side that can become stained giving the teeth a striped look.
Finally, the occlusion of the mouth. The upper and lower teeth fit together in a scissor bite. The teeth overlap but don't hit each other. This makes them brilliant for shearing through tough foods.
Cat dental chart
Any abnormality of occlusion can affect the 'self-cleaning' of your cat's mouth and increase the risk of dental disease.
What does 'dental disease' actually mean?
Most of the time when we say 'dental disease' we're actually talking about more than just the teeth. We're really talking about something called 'periodontal disease'. The word periodontium refers to the tissues that support the teeth and hold them in place (perio means 'around' and dontium means 'the tooth')
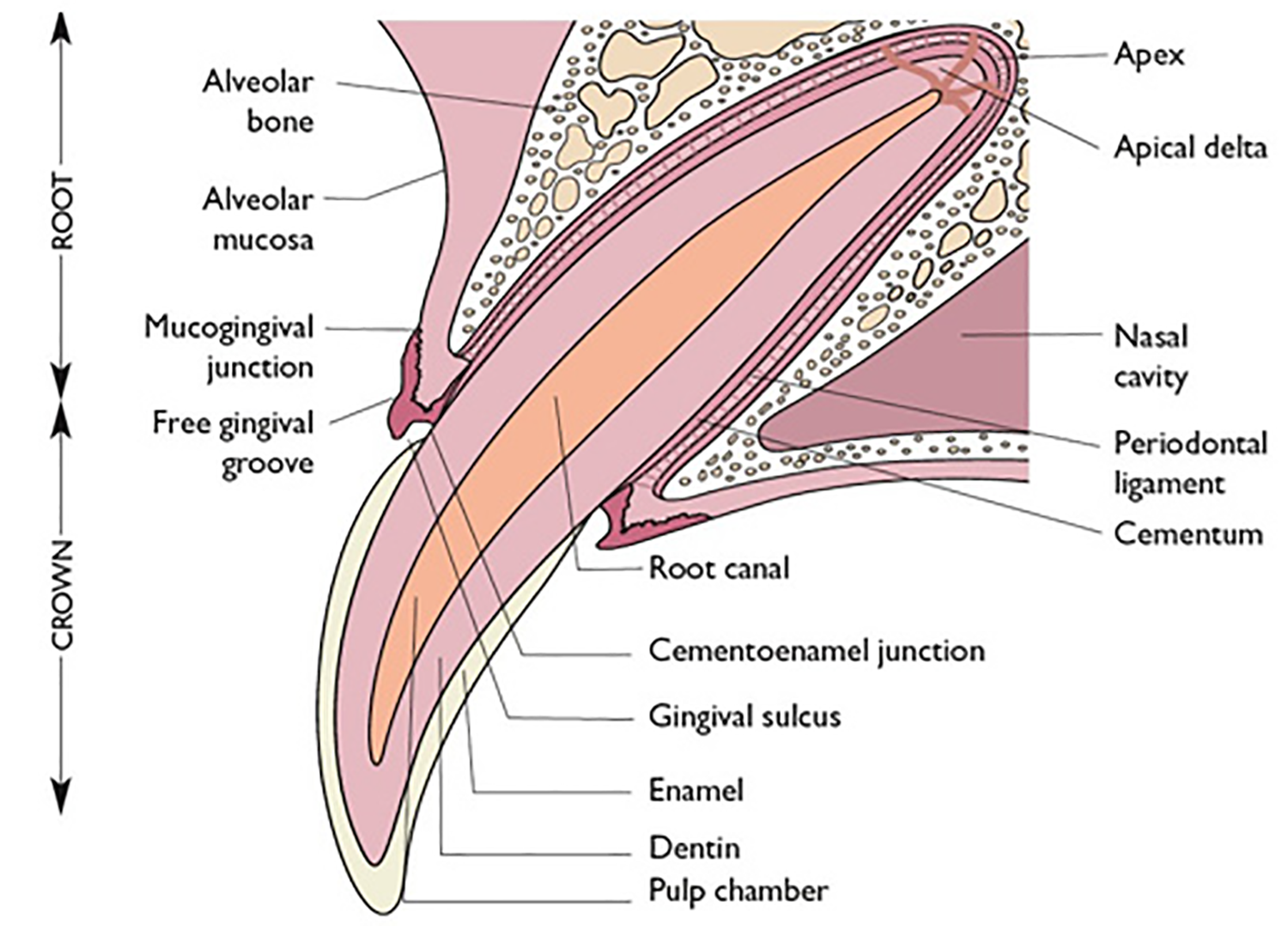
Cross section of a tooth
The periodontium is made up of:
- the gingiva (gums)
- the periodontal ligament (attaches the tooth to its socket)
- the alveolar bone (makes up the boney socket the tooth sits in)
- the cementum (bone-like stuff that covers the tooth root)
The gap between the tooth and the gum line (the gingival sulcus) is less than 1 mm deep in cats.
Periodontal disease starts when bacteria in the mouth mix with saliva to form plaque. This sticks to the surfaces of the teeth and if not removed, over time, it mineralises and becomes calculus (or tartar). Calculus sits on the tooth crowns, but plaque can get down below the gum line on the root surface of the teeth. There it can cause inflammation, infection and destruction of tissues. How bad these things are determines the stage of periodontal disease.
The bacteria and the decomposing periodontal tissue can result in some really hideous breath.
Stages of feline periodontal disease
There are four stages of periodontal disease:
- stage I is gingivitis, which happens when the plaque contacts the gums and the bacteria within it cause inflammation. You can see it as redness of the gums. Gingivitis is reversible.
- stage II is gingivitis plus the development of pockets between the gum and tooth, with plaque getting down under the gum line. This causes destruction of the periodontal ligament and alveolar bone and so the attachment of the tooth starts to loosen. Here we move to into irreversible stages of disease and likely tooth loss
- stage III means the pockets have deepened and there is advanced loss of periodontal ligament and alveolar bone (up to 50% of bone is lost at this stage)
- stage IV periodontal disease means there is greater than 50% bone loss and the tooth is obviously loose. This is end stage and the best treatment is extraction of the diseased teeth. With this amount of bone loss, there is an increased risk of jaw fracture and fistula (tunnel) formation between the mouth and the nose
It's difficult to accurately assess the stages of feline periodontal disease by just looking in the mouth. We really need to be seeing how deep the sulcus is with a probe. If the probe depth is more than 1 mm, then we've got at least stage II disease. Further assessment requires evaluating tooth mobility, gum recession and sometimes bone loss (with dental X-rays).
There are lots of different conditions that cause or are related to periodontal disease. We'll look at some of these next.
Pearly whites at the front don't always mean good teeth at the back
Common dental problems in cats
Juvenile onset gingivitis
As the adult teeth come through, it's normal for the gums to become a bit red and sore. This usually lasts a short time and once the new teeth are in (by 6 months of age), things settle down. But in some young cats the redness and swelling is more severe and it doesn't go away. This is known as juvenile onset gingivitis or juvenile hyperplastic gingivitis.
Affected cats have severe gingivitis and halitosis (stinky breath) but their teeth look clean. They can also be cranky cats due to the discomfort and may be very hard to give tablets to.
There has been a lot of research into this but, as yet, we don't know why it happens. It might be an exaggerated response to tooth eruption or due to exposure to a virus (eg feline calicivirus) or maybe it's an immune-mediated disease. We do know that it definitely occurs in some breeds more than others, with Main Coons, Siamese and Abyssinians commonly affected.
It can be difficult to treat. Cleaning the teeth, despite there being minimal plaque build up, can help. This may need to be done under general anaesthetic, with any persistent baby teeth being extracted and the gums treated to remove pocketing. At home cleaning is needed too. While tooth brushing is ideal, it's often too painful or just too difficult. Alternatives to brushing include dental diets, oral washes, water additives and dental treats. Drugs that work on the immune system have been used successfully in some cases.
Fortunately, juvenile onset gingivitis usually resolves by around 2 years of age.
Juvenile periodontitis
This is another inflammatory condition in young cats (less than 9 months of age). The gums are red and swollen, and bad breath is key sign, but it differs from juvenile gingivitis in that there is often plaque and tartar present, as well as bone loss.
It can occur in any cat, but some pure breeds seem to get it more (eg Siamese, Burmese, Abyssinian, Himalayan).
Juvenile periodontitis is treated in the same sort of way as juvenile gingivitis with home and and in-clinic teeth cleaning. But tooth extractions are frequently needed (due to the bone loss). Some cats do seem to grow out of it, although they tend to require more frequent dentals throughout their lives than unaffected cats. Unfortunately for some other cats, the disease persists. These cats may need all or almost all of their teeth out to control the symptoms.
Tooth resorption
You can think of tooth resorption like 'cat cavities'. And it's is a very common condition – occurring in up to 75% of cats. The cavities (or lesions) are where the tooth is sort of being dissolved.
The lesions can appear on any surface of any tooth, but are most common on on the outside of the premolar of the lower jaw. The tend to occur near the gum line, which is why they used to be called 'neck lesions' (occurring at the neck of the tooth). Sometimes it looks like the gum is growing down the tooth.
The lesions vary from mild (small holes in the tooth surface) to severe (where the crown of the tooth has broken off due to weakness and the gums have grown over the tops of the roots).
Despite a lot of research into feline tooth resorption, we're not sure why it happens. Recent studies suggest there are two types of resorptive lesions, which can be distinguished with dental X-rays:
- type 1 – is associated with periodontal disease
- type 2 – is associated with bone replacement
The reason we need to know about these types is that type 1 needs the affected teeth to be completely extracted and type 2 can be treated by removing the crown and leaving the roots.
Stomatitis
The term 'stoma' means mouth or opening, and when you add 'itis' – you get inflammation. So stomatitis is inflammation of the mouth. This doesn't sound so bad, but stomatitis is awful – it's painful for the cat and frustrating for the people caring for the cat.
Affected cats have bad breath and bad gingivitis. But the inflammation doesn't just stay around the teeth, it spreads to the back of the mouth, the roof of the mouth and the throat. Due to the pain, these poor cats often drool, don't eat and can't groom themselves. They can be really miserable – imagine having a mouth full of ulcers and you're probably in the ball park.
It appears to be an immune-mediated reaction to either plaque or to the tooth itself. There are several factors involved such as genetics, stress, diet and viral infections (eg feline calicivirus). As far as genetics go, Himalayans, Persians and Somalis seem to be the most affected.
Stomatitis is generally pretty easy to diagnose on history and examination. But sometimes, especially when we don't know when the problem started, we can't tell by just looking if we have stomatitis, an allergic reaction or even cancer in the mouth. If this is the case, we might take a biopsy or do a trial of some treatment.
When biopsies of the inflamed tissues are taken, the pathology report will often say: 'lymphocytic, plasmacytic' stomatitis. Lymphocytes and plasma cells are white blood cells and part of the immune system.
Although extracting the teeth is a key part of therapy, there isn't really a one-size-fits-all treatment for stomatitis. Medical, surgical or a combination of the two might be needed. A lot depends on how bad it is and well the cat can cope.
Medical treatment tends to involve antibiotics and anti-inflammatories (eg cortisone). It does tend to work well in the short term. Long term, not so much. Additional pain medication can also help.
Surgical treatment involves meticulously removing affected teeth and remnants of teeth. As these can be hidden below the gums, dental X-rays are usually needed. Leaving any bits of tooth root behind keeps the inflammatory process going and defeats the purpose of treatment. We'll often remove some of the inflamed gum too, as bacteria can hide out in inflamed tissue and, again, keep the inflammation going.
While these cats are healing, they may need to be fed through a tube that bypasses the mouth and goes into the food pipe (oesophagus).
How can I tell if my cat has dental problems?
All of those diseases can be rather confusing, but when it comes down to it, most cat dental problems present in much the same way. If you notice stinky breath (halitosis) or red gums (gingivitis), your cat might have dental disease.
Other signs include:
- broken teeth
- excessive drooling
- reluctance to eat, particularly harder foods
- not grooming
- pawing or rubbing at the mouth
- bleeding from the mouth
If you're not sure what you're looking at (or smelling) then our nurses are happy to do a free dental check for you.
See this cat's higgledy piggledy lower incisors?
Can I prevent dental disease?
Maybe. As you've seen, genetics play a role in feline oral disease, so there's not much you can do about that. But good dental hygiene also plays a major role. You might be able to prevent a lot of dental problems with dental diets, dental products and daily brushing, but just feeding biscuits probably won't do the trick.
Some animals have beautiful teeth their whole life. Others need help keeping their chops clean. This help often comes in the form of a 'dental', which is a clean and polish under general anaesthetic.
What happens during a dental?
During a dental all calculus is removed and every tooth is examined and probed for signs of periodontal disease. Using an ultrasonic scaler, plaque is removed from the surface of both the crowns of the teeth and the roots.
Teeth that are unable to be saved are removed. We never remove healthy teeth! Extracting healthy teeth is actually really hard to do and we're not interested in making things harder than they need to be. Sometimes we'll use dental X-rays to help us decide if the teeth are saveable or not.
Depending on which teeth are removed, we may close over the hole with sutures or leave it open to heal. The good thing about the mouth is that is has a great blood supply and usually heals very quickly – most wounds are pretty good within about 3 days!
After each side of each tooth is cleaned, all the teeth are polished.
We only perform dentals when the benefits of the procedure outweigh the risks.
Do you do anaesthesia-free dental cleaning?
No we don't.
We perform dentals under a general anaesthetic. This allows us to:
- thoroughly examine your pet's entire oral cavity
- clean each side of each tooth, including up under the gum line
- take dental X-rays to look for problems with tooth roots and the jaw bones
- remove loose, rotten or fractured teeth if needed
No one is suggesting that anaesthesia doesn't involve some risk. However, even for older pets, the risk is low with today's anaesthetics. We tailor anaesthetic techniques for each pet and minimise risks with high-quality monitoring and support (eg IV fluids). We can also run blood tests before any procedure to look for things like kidney and liver disease, which can affect anaesthetics.
There are places that offer anaesthesia- or sedation-free dental cleaning. If you are interested trying this for your cat, questions to ask include:
- Do you clean all sides of every tooth?
- Do you clean below as well as above the gum line?
- Do you probe around the teeth to check for pocketing and areas of attachment loss?
- If extractions are needed, can you do this and who will do this?
If you want more information, please talk to us!